Abstract
Introduction
Immune thrombocytopenia (ITP) in children typically manifests with acute, severe thrombocytopenia leading to variable mucocutaneous and tissue bleeding. Despite gaining insight into disease biology, there is no confirmatory diagnostic test, leaving the clinician to exclude other causes of thrombocytopenia through clinical and laboratory findings. The immature platelet fraction (IPF) is determined by hematologic analyzers via platelet size and RNA content and serves as a measure of bone marrow thrombocyte production. A higher value indicates increased thrombopoiesis. While data exists regarding the validity of IPF as a diagnostic tool for differentiating hypo-productive and consumptive etiologies of thrombocytopenia in the adult population, there is a paucity of data regarding its use in the pediatric population.
Objectives
This study set out to determine how the IPF value may be utilized to support the diagnosis of ITP among pediatric patients.
Methods
This is a retrospective cohort study at a single tertiary care children's hospital. The electronic medical record (EMR) system was reviewed to include all patients who had an IPF resulted from January 1, 2016 through December 31, 2021. The investigators utilized REDCap ® (Research Electronic Data Capture) to create a database of pediatric patients with thrombocytopenia including their laboratory findings and final diagnoses.
Patients were classified as either ITP or non-ITP. Characteristics of ITP and non-ITP cohorts were compared using Wilcoxon rank sum test and Pearson Chi-square test. An ROC-AUC analysis was conducted to identify the IPF value which best predicted if the patient had ITP or not with a 95% confidence interval (CI). The optimal cutoff value was estimated using Youden's index. Sensitivity and specificity were estimated for the cutoff value. Univariable logistic regression was then used to estimate associations between patient characteristics and diagnosis of ITP. Multivariable logistic regression was used to estimate the association between binary IPF and ITP adjusting for other predictors. Statistical significance was assessed at the 0.05 level.
Results
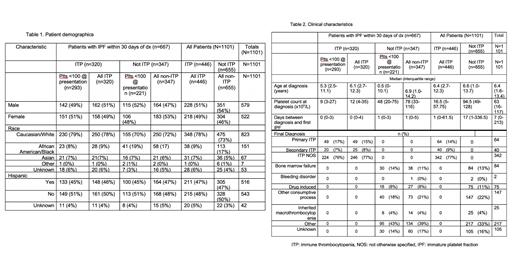
Demographics shown in Table 1 are stratified by patients who had their IPF within 30 days of diagnosis of thrombocytopenia and those who did not. The IPF was significantly higher at presentation in all patients with ITP than patients without ITP (median IPF 12.8% vs 10.5%, P=0.018). An optimal IPF cutoff point for ITP vs. not ITP among all patients was determined to be 5.4% with a sensitivity of 0.85, specificity of 0.39, and AUC of 0.623 (95% CI: 0.527, 0.718). The platelet count for patients with ITP was significantly lower at presentation than in patients without ITP (median 16 x 10 9/L vs 86 x 10 9/L, P<0.001). Logistic regression modeling using IPF as a binary variable, either >5.4% or not, showed that IPF >5.4% is significantly associated with ITP (P<0.001). Platelet count at presentation was also significantly associated with a diagnosis of ITP (P<0.001) and a single unit increase in platelet count decreased odds of ITP by a factor 0.98 (95% CI: 0.97, 0.99). After adjusting for platelet count, IPF >5.4% was still significantly associated with ITP (P=0.003). Those with an IPF >5.4% were 3.34 times more likely to have ITP than non-ITP (95% CI: 1.49, 7.31).
When the population was adjusted to include only patients with a platelet count of <100 x 10 9/L at presentation and those that had an IPF obtained within 30 days, the optimal cutoff point for IPF was 15% with a sensitivity of 0.46, specificity of 0.80 and AUC of 0.58 (95% CI: 0.458, 0.719).
Conclusion
The data demonstrates that in thrombocytopenic patients, a high IPF (>5.4%) is associated with ITP, but the sensitivity for predicting ITP is low.
Despotovic: Apellis: Consultancy; Agios: Consultancy; Novartis: Consultancy, Research Funding; UpToDate: Patents & Royalties: Royalties. Kirk: Biomarin: Honoraria.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal